Cancer and severe pain led Michigan’s list of qualifying conditions when the state legalized medical marijuana in 2008. More than a decade later, cancer and severe pain patients should have easy access to medical cannabis products—but that’s not the case.
'Dogs have easier access to medical cannabis than cancer patients.'
In fact, those with the greatest medical needs face the biggest obstacles to obtaining high-quality medical cannabis products—and accurate information about how to use them.
“Dogs have better options [for medical marijuana] than cancer patients right now,” observes one dispensary owner. That owner, who I’ll call Adam (he requested to be anonymous due to his pending business application with the state), is both a retired veteran and a cancer survivor himself.
Technically speaking, he may be correct. Companies like Canna Companion make medicinal CBD products for dogs and cats that are easily available online. Meanwhile, Michigan’s medical patients have to hunt for doctors willing to write them a recommendation, for caregivers or dispensaries where they can find products (a one-to-three-hour drive for many residents), and for personalized information about dosages and use.
“When you’re a cancer patient looking to go the cannabis route, you’re treated like a second class citizen,” says Adam.
It’s Tougher for Older Adults

Ruth Ann Steele, 70, in her bedroom at her home in Big Rapids, Mich., on Thursday, January 24, 2019. Steele does not smoke marijuana but uses CBD creams and products for pain. (Brittany Greeson for Leafly)
While medical patients of all ages face these same obstacles, older adults typically lack the knowledge about cannabis, connections to the industry, and digital-native research skills that younger medical patients enjoy. That makes it very difficult for seniors to access good meds and good info. Senior cancer patients, says Adam, “are apprehensive because they’ve had no chance for education about cannabis. They’re starting like they’re two years old.”
Still, despite the difficulties, many pain and cancer patients older than 55 are seeking cannabis. And they’re overcoming old fears and stereotypes they’ve been fed for their entire lives.
My own mother recently offered her personal experience as an example.
Mom Asks: Why Didn’t We Do This Earlier?

Family photos, books and memorabilia sit on a piano at the home of Ruth Ann Steele, 70, in Big Rapids, Mich., on Thursday, January 24, 2019. Steele does not smoke marijuana but uses CBD creams and products for pain. (Brittany Greeson for Leafly)
“The more we learn, the more we realize [cannabis prohibition] was a bill of goods,” she told me. Mom—aka Mecosta County resident Ruth Ann Steele, 70—has watched her mother, sister, niece, cousin, brother-in-law, and husband die from cancer over the past 15 years. None of them had knowledge of or access to medical marijuana. Her perspective on the subject of cannabis has shifted significantly over the last few years, especially since her husband lost the battle to melonoma in 2007.
Shop highly rated dispensaries near you
Showing you dispensaries near“At the time [2007], I would have laughed,” she told me. “We didn’t know anything, other than it was a hippie high. Medicinal qualities to cannabis? No, we didn’t know anything about that. But the cannabis industry has been so demonized. We want nothing to do with it because it’s been so stereotyped. But when you watch TV—how many of those commercials are for drugs? It’s just astounding. We desperately need something other than big pharma.”
Holly: Battling Cancer with Little Info
My mother’s friend Holly (a pseudonym) is a 62-year-old resident of Michigan’s Upper Peninsula. Cannabis is nothing she would have ever considered consuming—until recently.
A wife, mother of five, and grandmother with deep religious convictions, Holly is opposed to “deliberately denying oneself of one’s reason”—i.e., bringing about a state of intoxication.
When her leukemia diagnosis came in, Holly began researching the medical uses of cannabis. That information convinced her that it needed to be part of her treatment. This was thanks in part to her two brothers, who both use cannabis medicinally. They encouraged her to do the same.
“I’m not interested in the psychoactive effects,” Holly told me. “But there seem to be so many benefits to using this plant. Once I was assured I wouldn’t have to get high, I was on board.”
Recommendation, Then You’re On Your Own

Snow covers colonial style homes in downtown Big Rapids, Mich., on Thursday, January 24, 2019. (Brittany Greeson for Leafly)
Although Holly’s family practitioner was willing to write her a recommendation for her medical card, nobody at the clinic was able to give her any information about where to get the product, and what kind of dosage she should take.
Similarly, Holly’s oncologist at a leading cancer research hospital noted that most of their Colorado and Michigan-based patients are using marijuana—but they offered no information regarding the best delivery and dosage.
“The biggest barrier is finding someone who’s knowledgeable about the plant, and about dosage,” says Holly. “How many milligrams should I take? What is the right route, and the right material?”
The nearest dispensary is a two-hour drive from Holly’s home. Although she’s been successful in sourcing product from a caregiver locally, she has yet to be able to access cannabis in forms beyond smoking or vaping flower. She’s currently making her own tinctures—a three week process.
Vaporizing, but Is That Best?
Holly is uncomfortable with smoking due to the potential psychoactive effects. So she’s been vaporizing, and has been enjoying relief from nausea and some of the pain. But she knows she’s not making full use of the plant’s medicinal capabilities. She knows she needs more information and a more targeted product.
When you’re sick like this, you just want somebody to say ‘Here, do this.’
How cannabis is delivered, as many budtenders and caregivers know, can have a huge impact on its results.
“Cannabis is the Swiss army knife of medicine,” says Adam, the dispensary owner. “We tell every cancer patient: Your own personal experience affects you differently than others. If you have access to the right meds, you won’t have to worry about negative side effects. The quality of the medicine is really the driving factor.”
With no budtenders or dispensaries around for 100 miles, accessing the best delivery system is difficult for Holly. And that’s frustrating.
“There are so many things to deal with in this type of situation,” Holly tells me. “When you’re sick like this, you just want somebody to say ‘Here, do this.’”
Holly’s biggest goal in using cannabis is to decrease her daily dose of morphine, which is currently at 45mg. She’s concerned not only about morphine’s psychoactive effects, but the long term consequences of taking opioids.
Ron: Cannabis for Opioid Recovery

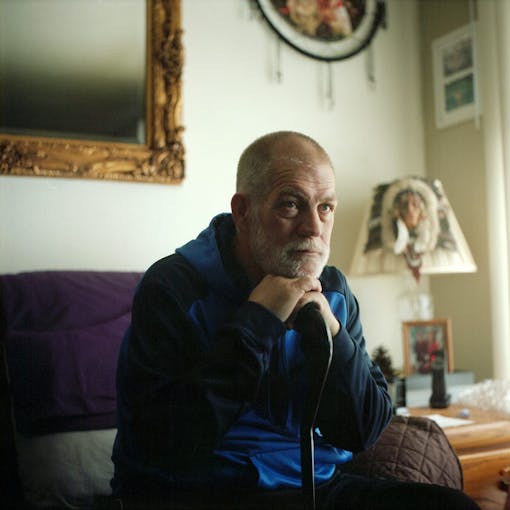
Ron Morris, 62, prepares to use his marijuana vaporizer at his home where he lives with his wife in Kalamazoo, Mich., on Wednesday, January 23, 2019. Ron got his medical card the year after it first became legalized in the state of Michigan. (Brittany Greeson for Leafly)
Ron Morris is a 62-year-old pain patient and retired 82nd Airborne paratrooper. “I found cannabis in spite of the doctors’ help,” he says. “I was taking four 750mg Vicodins a day, every day, for about eight years. When I quit taking them, the pain stayed the same. The only thing they were doing was making me believe I was doing something for the pain.”
'The first time I vaporized cannabis, the pain went away. I didn’t care about the stigma—all I could think was that I didn’t hurt anymore.'
Morris had also been on 500mg per day of Naproxen for 10 years, to help manage his knee and back pain from the compression injuries he incurred during his service.
“They’re only supposed to prescribe that for up to 30 days, but they were giving it to me for 10 years,” Morris says. He lists stomach ulcers among his other symptoms, as well as PTSD from his active duty days.
“The first time I vaporized cannabis, the pain went away,” Morris recalls. “I didn’t care anymore about the stigma, or any of that—all I could think was that I didn’t hurt anymore.”
‘Dad, You Need to Try This’

Photos of Ron Morris, 62, and his grandson hang on the fridge of his home where he lives with his wife in Kalamazoo, Mich., on Wednesday, January 23, 2019. Ron got his medical card the year after it first became legalized in the state of Michigan. (Brittany Greeson for Leafly)
Morris discovered cannabis from his son, who had a medical license to manage shoulder pain from his manual labor job. His son begged Morris to try his vaporizer.
“I said, ‘I’m high enough on this stuff,’ and he said, ‘Dad, this is totally different.’ So one day I was in absolute pain, and I said OK.” Morris said he didn’t notice any immediate effects—not until he came back from the bathroom and his wife noted that he was standing straight up for the first time in years.
“It used to be, you get up, take your meds, then turn into a zombie,” Morris recalls. “But now, I get up and get around in the morning. You can’t believe what a big world it was out there, after ten years of that.”
After a few days of his medical cannabis treatments, Morris returned a full bottle of Vicodin to the VA.
Elizabeth: Back Pain Relief

Elizabeth Ouding at her home in Kalamazoo, Mich., on Wednesday, January 23, 2019. Ouding, who uses marijuana to treat pain from a back surgery and other ailments, will soon be starting a job at a local dispensary and hopes to educate customers about marijuana products to treat chronic pain. (Brittany Greeson for Leafly)
Elizabeth Ouding, 51, took refuge in cannabis after being sent on a complicated hunt to refill the pain medication her surgeon had put her on after back surgery. After the sixth such surgery (the last of which was to correct an injury incurred by the fifth surgery), her surgeons placed her on heavy pain narcotics.
'If I don’t use the cream, or smoke or eat something, I can’t move. It helps with depression, too—that should be noted.'
“The doctor who did the surgery informed me he could no longer prescribe the narcos, I had to go to my family doctor,” Ouding recalls. “Of course, then she told me she couldn’t prescribe them because she didn’t do the surgery. So they tried to send me to a pain clinic.”
Meanwhile, Ouding was going through severe withdrawal from the narcotics she’d been prescribed for previous surgeries. “For two weeks I was lying on my couch sweating, and thinking I was going to die.” She told her husband she’d rather experience the excruciating pain than go through withdrawal again.
She managed to get a recommendation for medical marijuana, and went to her nearby dispensary in tears. “I’m telling him no narco. That I’m dying going through withdrawals. So he gave me a little to smoke, gave me some edibles, gave me the capsules—those are amazing. I take one of those 100mg CBD+THC capsules in the morning, I’m good all day.”
Ouding says if it wasn’t for cannabis, she couldn’t function. “If I don’t use the cream, or smoke or eat something, I can’t move. It helps with depression, too—that should be noted.”
Veterans: Sorry, No Help at the VA

A mural depicting an industrial scene of the logging industry is seen in downtown Big Rapids, Mich., on Thursday, January 24, 2019. (Brittany Greeson for Leafly)
When Ron Morris asked his doctor at the Veterans Administration for a medical marijuana recommendation, she turned him down and told him to go get his medical card elsewhere—without providing any referrals.
Eventually Morris found Dr. Thomas Crocker’s Michigan Holistic Health practice in Lansing. “He was a real doctor,” Morris emphasizes. “He knows his stuff about cannabis and the medical benefits. He gave me a real physical, and he wrote me my card.”
This has been one of the pinch points for patients in Michigan’s medical marijuana program. A patient must have a doctor’s recommendation in order to qualify for a medical card. But due to strict hospital regulations, lack of education in the medical community, and insurance liabilities, few hospital or family doctors have been willing to write marijuana recommendations for their patients.
They are often left to their own devices to seek out a private practitioner who understands and is comfortable with cannabis. But for many in the boomer and silent generations, the legitimacy of having their own authoritative practitioner write the card seems to be particularly important. Even raising the subject with a longtime family doctor can be terrifying.
“There is a fear when you go to your medical doctor,” my mother tells me. “Because they sit on the right hand of God. You can’t not do what they tell you, which includes the chemo regimen and everything else, even when they’re telling you they have no cure for it.”
Most Mainstream Docs Won’t Touch It

Elizabeth Ouding demonstrates how she rolls a joint at her home in Kalamazoo, Mich., on Wednesday, January 23, 2019. Ouding, who uses marijuana to treat pain from a back surgery and other ailments, will soon be starting a job at a local dispensary and hopes to educate customers about marijuana products to treat chronic pain. (Brittany Greeson for Leafly)
None of my mother’s family members were offered cannabis by any of their doctors during their battles with cancer. Medical marijuana has been legal and available in Michigan for ten years—but patients like Mom’s brother-in-law, who died within the last two years, were never offered the option.
“Cancer patients are most discriminated against by their own doctors,” says Adam. “There’s no education or information about cannabis. Doctors are mandated to be advocates for their patients—so where is the advocacy? They’re scared of cannabis because hospitals rely on federal grant funding.”
It’s true that most hospitals often rely on considerable grant funding, and that both hospitals and private practices also rely on income from federal Medicaid and Medicare programs. Organizations which receive federal funding are required by both the terms of these programs and by insurance policies to follow federal policies—including the federal government’s continued prohibition and classification of cannabis as a Schedule I controlled substance, verboten in any clinical setting.
Vets in Federal Housing: No Cannabis Allowed
Ron Morris, 62, at his home where he lives with his wife in Kalamazoo, Mich., on Wednesday, January 23, 2019. Ron got his medical card the year after it first became legalized in the state of Michigan. (Brittany Greeson for Leafly)
Residents of federally subsidized housing face a similar conundrum—including many formerly homeless veterans who have received housing through HUD, a federal agency.
“Other veterans “see me and talk to me and want [medical cannabis] so bad,” says Ron Morris, “but a lot of them are living at the Gold Star House, so the best thing they can do is get someone to give it to them.”
Indeed, HUD’s memos from 2011 and 2014 on the subject require property managers of assisted or public housing to deny applications for housing if the applicant is actively using medical marijuana. The memos leave it up to the owners to decide whether or not to evict a resident who has been found using medical marijuana after they’ve become a resident. Dennis Sturtevant, CEO of The Dwelling Place, which manages thousands of federally subsidized housing in Grand Rapids and across the state, says this puts owners in an untenable position “that will eventually result in a court challenge that will result in more clarity on this issue.”
Sturtevant says he expects this situation to change in the near future, as a majority of states legalize marijuana.
More Clinics for Patients
In the meantime, a growing number of pioneering private practitioners are becoming friendly to marijuana, and rising to meet the huge demand for alternative pain treatment. Dr. Marla Gendelmen, an anesthesiologist with a pain practice in Norton Shores, told the South Bend Tribune earlier this year that cannabis is “a lot safer than narcotics, and in many ways it’s safer than Aleve.” She observed that “when you look at the long-term side effects of taking non-steroidals [like ibuprofen], turns out they’re not benign.”
Gendelman also pointed out that marijuana “doesn’t create physical dependence like an opioid.”
Grand Rapids practitioner Dr. David Sova offers marijuana prescriptions as part of his practice’s suite of pain management and counseling services. He’s considering opening a dispensary in Grand Rapids’ neighboring Cascade Township. That would give his clients easier access to medication, as Grand Rapids’ nearest dispensary is a one-hour drive away in TK TOWN).
Time for a Culture Change

A thin sheet of ice covers a lake outside of Kalamazoo Mich., on Thursday, January 24, 2019. (Brittany Greeson for Leafly)
Although Elizabeth Ouding still faces more back surgeries, she has peace of mind about her pain management regimen. She no longer fears getting caught in the opioid cycle.
“I wish I could get this message out to people stuck on opioids, because I know why they’re stuck,” she tells me. “When they start to go in that withdrawal stage, they get stuck, and they get in for more. And if it wasn’t for Adam helping me, and my husband, I wouldn’t have made it through.”
Morris echoes Ouding’s passion for changing the culture and erasing the stigma of cannabis for older patients. “I was living a life for about 10 years that just…wasn’t any way to live,” he says. “That’s why I went to the mental health people—because I was about to end it. And now I’m totally out of the woods. I can get up and go out in the morning, and if I come home and hurt, I smoke a bit, then I don’t hurt, and I can go out to dinner with my wife.”





